A Case Report of Facial Swelling and Crepitus Following a Dental Procedure
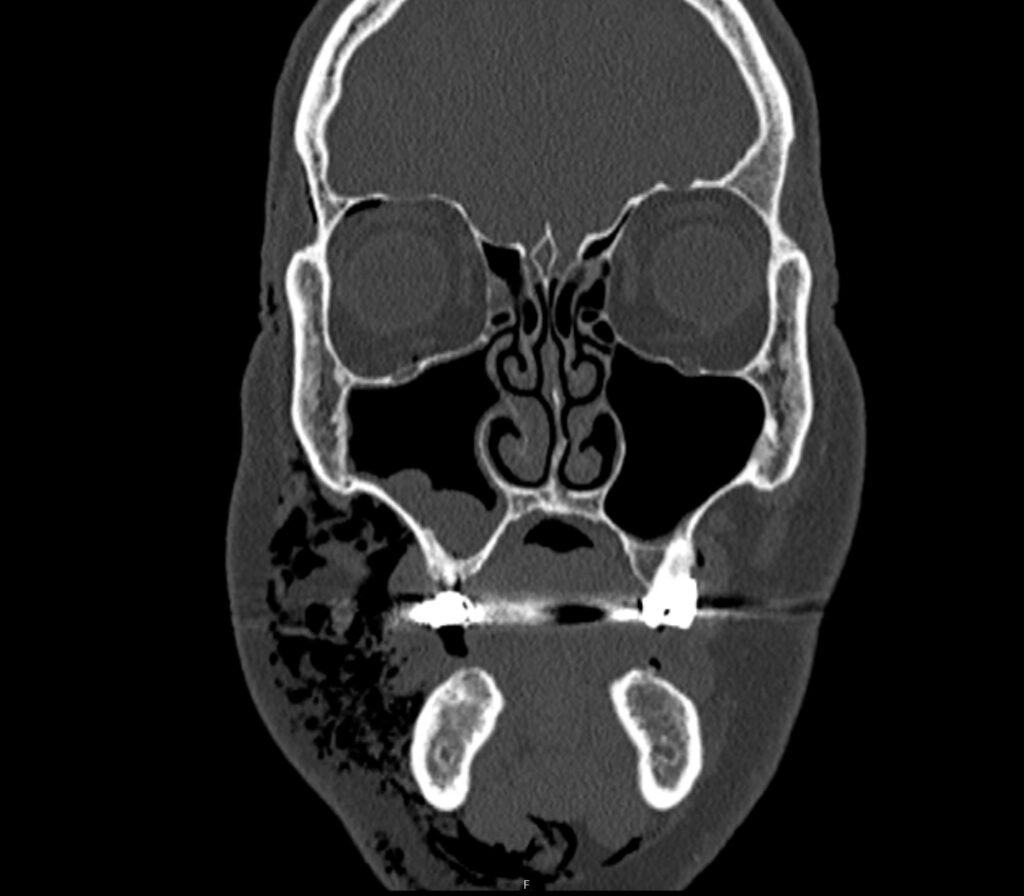
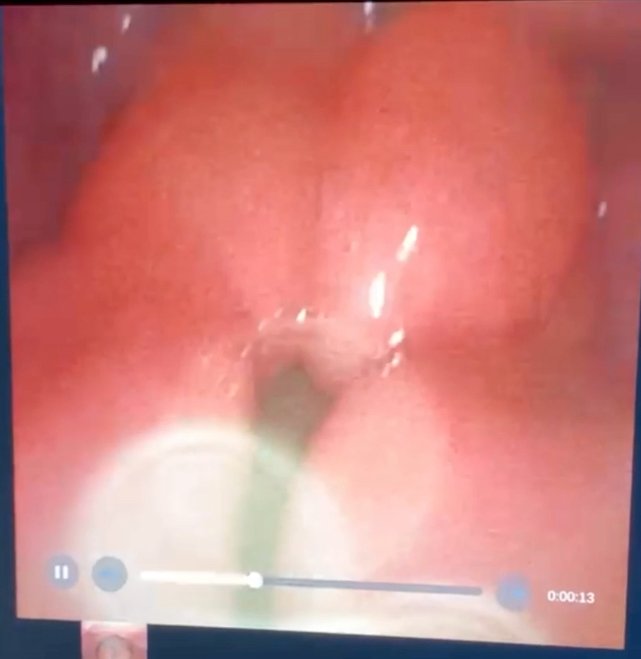
Given the physical exam findings of crepitus on the right neck up to the right lower eyelid, a maxillofacial CT scan without contrast was performed. It revealed diffuse subcutaneous air within the soft tissues of the face and neck and free air within the pre-septal soft tissue of the right eye, appearing as hyperlucent (dark) areas on CT within the soft tissue planes (blue outline). It showed no evidence of post-septal free air. A single-view chest X-ray was also performed and was unremarkable except for incompletely imaged soft tissue gas in the right lower neck (blue outline). On flexible fiberoptic laryngoscopy performed by ENT, the oropharynx appeared diffusely edematous and narrowed.