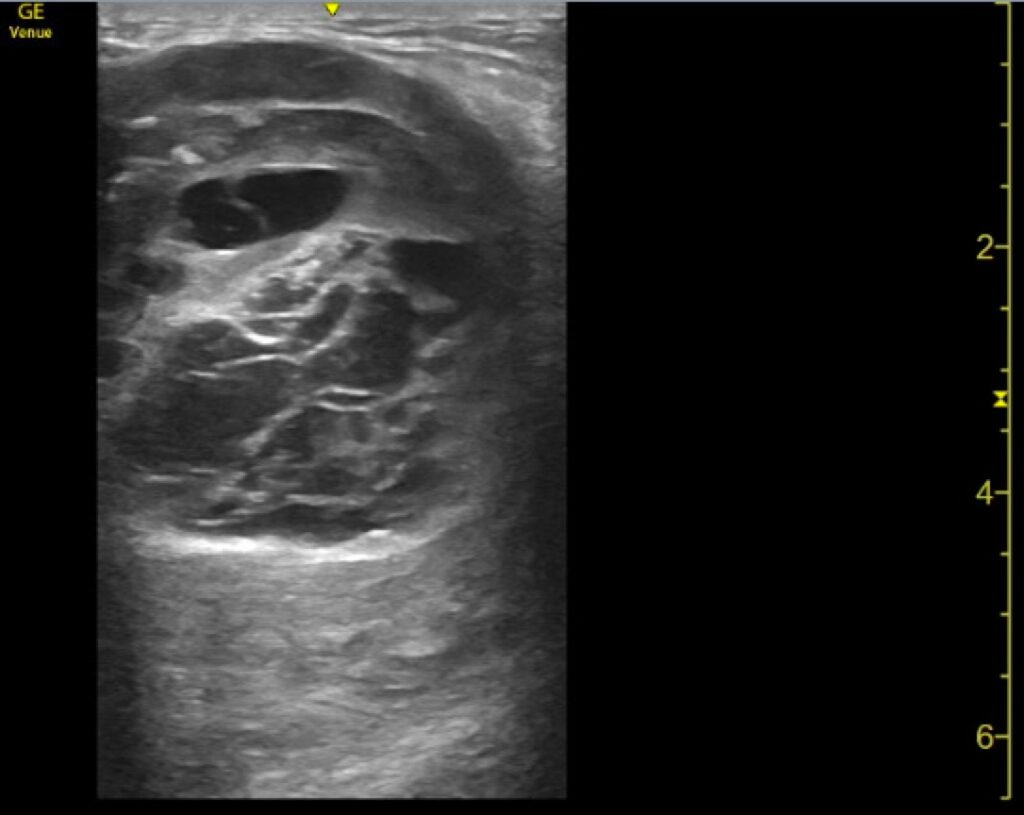
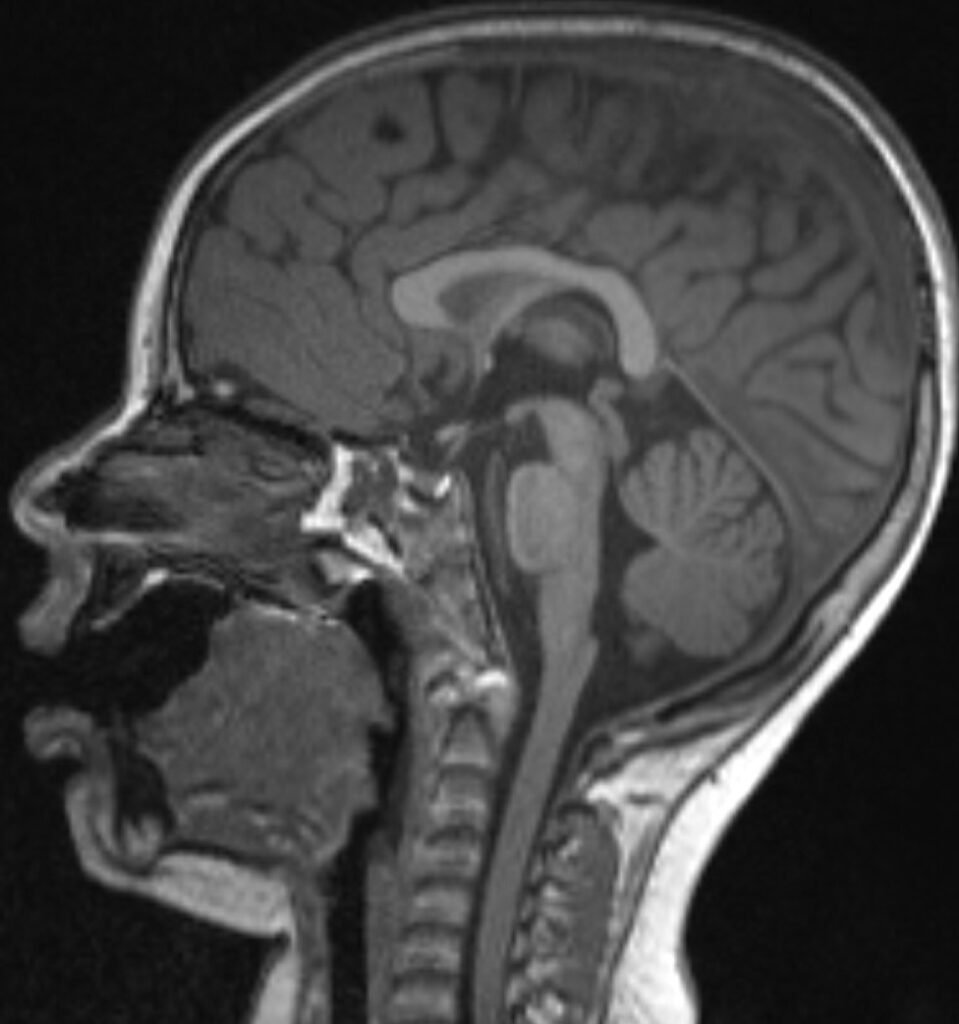
After completing this simulated case, participants will be able to: 1) Obtain a detailed history that includes recent medications, medical, surgical, and social history to evaluate for HIT risk factors, 2) perform an adequate neurovascular exam including evaluation of motor function, sensation, skin color, pulses, and capillary refill, 3) order appropriate laboratory testing and imaging for diagnosis of thrombocytopenia and arterial occlusion, including bed side doppler or ultrasound, 4) discuss and recognize the symptoms of HIT and the contraindications of platelet and heparin administration in the emergency department, 5) avoid administration of heparin in the emergency department setting and recognize that platelets may worsen thrombus formation and lead to limb amputation, 6) select appropriate medications for treatment and determine appropriate disposition for a patient presenting with HIT, 7) demonstrate interpersonal communication with patient and family, 8) recognize that HIT with thrombosis is a potential complication in hospitalized patients and outpatient settings and is associated with high mortality rates.